Implantable iPSC derived liver and pancreatic cells: the future of medicine?
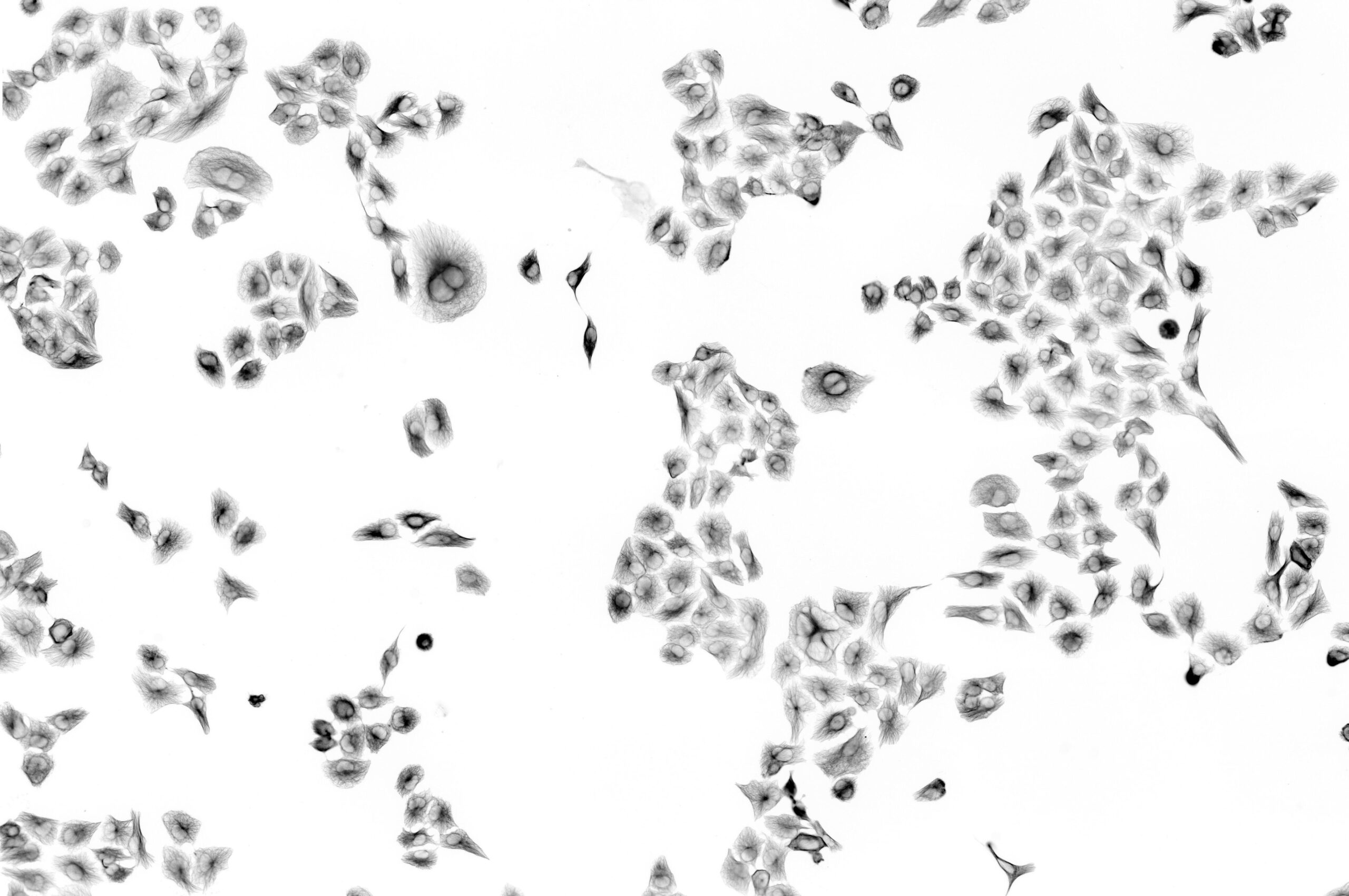
Endoderm implants combine synthetic support structures and cells to repair or replace the function of endoderm-derived organs like the pancreas, liver, colon, stomach, intestines, lungs, and gall bladder. Adult cells are notoriously difficult to expand in vitro without loss of function, so many implants have harnessed new technologies based on induced pluripotent stem cells (iPSCs) and embryonic stem cells (ESCs). Pioneers in the field are working to optimize cell lines and effectively scale manufacture protocols to transition to the clinic and fulfill the promise of these next generation of stem cell therapies.
Few therapeutic options are currently available for type 1 diabetes. The administration of exogenous insulin is a transient remedy which is burdensome on the patient, whilst cadaver-derived islet cell transplants are limited by donor availability and long-term effectiveness. Pancreatic implants are the most advanced therapeutic endoderm implant, with several devices progressing to clinical trials. The ongoing phase 1/2 trial by Ramzy et al and Shapiro et al based on a previous clinical study, use pluripotent stem cell-derived pancreatic endoderm cells housed in macroencapsulation devices, with ports to allow vascularization of the device providing direct support to the cells. Although immunosuppression is critical for this type of approach the study has already reported improvements in patient quality of life, with evidence of meal-induced secretion of insulin by differentiated stem cells in patients. To mitigate immune rejection, HLA-typed iPSCs could be used in future iterations of the device, although the risk of an immune response to minor antigens is still being investigated.

Patients with liver failure also have limited therapeutic options, with transplantation still being the only cure for irreversible liver failure. Although living donor transplants are possible thanks to the regenerative capacity of the liver, there is still a massive disparity between demand and availability. Stimuliver, a University of Edinburgh spin out created through the Venture Lab acceleration program at the BioInnovation Institute in Copenhagen, is tackling this problem with research into iPSC-derived liver tissue from David Hay’s CRM labs.
“The generation of implantable human tissue to treat debilitating disease is of paramount importance. We have generated proof of concept that human liver tissue can be deployed underneath the skin and supports recipient organ function from a far. These capabilities are the focus of Stimuliver, which generates human liver tissue implants at clinical grade.” – Professor David Hay, CEO of Stimuliver
The EMA and FDA are implementing regulatory guidance for many stages of development of complex cell therapy combined products. Raw, or ancillary materials used in the manufacture of stem cell therapies have a major impact on the characteristics, safety and success of cellular products. Transitioning manufacture processes to highly chemically defined, animal-free growth factors, proteins and culture media, which are manufactured according to cGMP guidelines provides cell therapy developers the best chance of a smooth transition to clinical phases.
There is enormous potential for next generation stem cell derived allogeneic cell therapies to relieve the global healthcare burden that we have today from diseases such as liver failure and diabetes. With optimized cell sources and matrices supported by the availability of high-quality raw materials, these lifesaving treatments can be delivered to patients.
Find the perfect proteins for your chemically defined iPSC and ESC media at Qkine